Sunstone Spotlight
Here we share with you all things related to the diagnosis, treatment, and care of our beloved pets. Check back often as there is always something new to learn. If there is a particular topic you are curious about, let us know and we may just include the answer in a future blog post.

Emerging News, Pet Safety, Sunstone Updates, Tests and Procedures
Scheduling your pet’s Internal Medicine Consultation at Sunstone Veterinary Specialists is an important step in ensuring they receive expert care for complex medical issues. Our goal is to...

Sunstone Updates, Tests and Procedures
CCL Tear in Dogs: Causes, Symptoms, and Treatment A CCL tear in dogs is one of the most common causes of hind leg limping. The Cranial Cruciate Ligament...
Sunstone Updates, Tests and Procedures
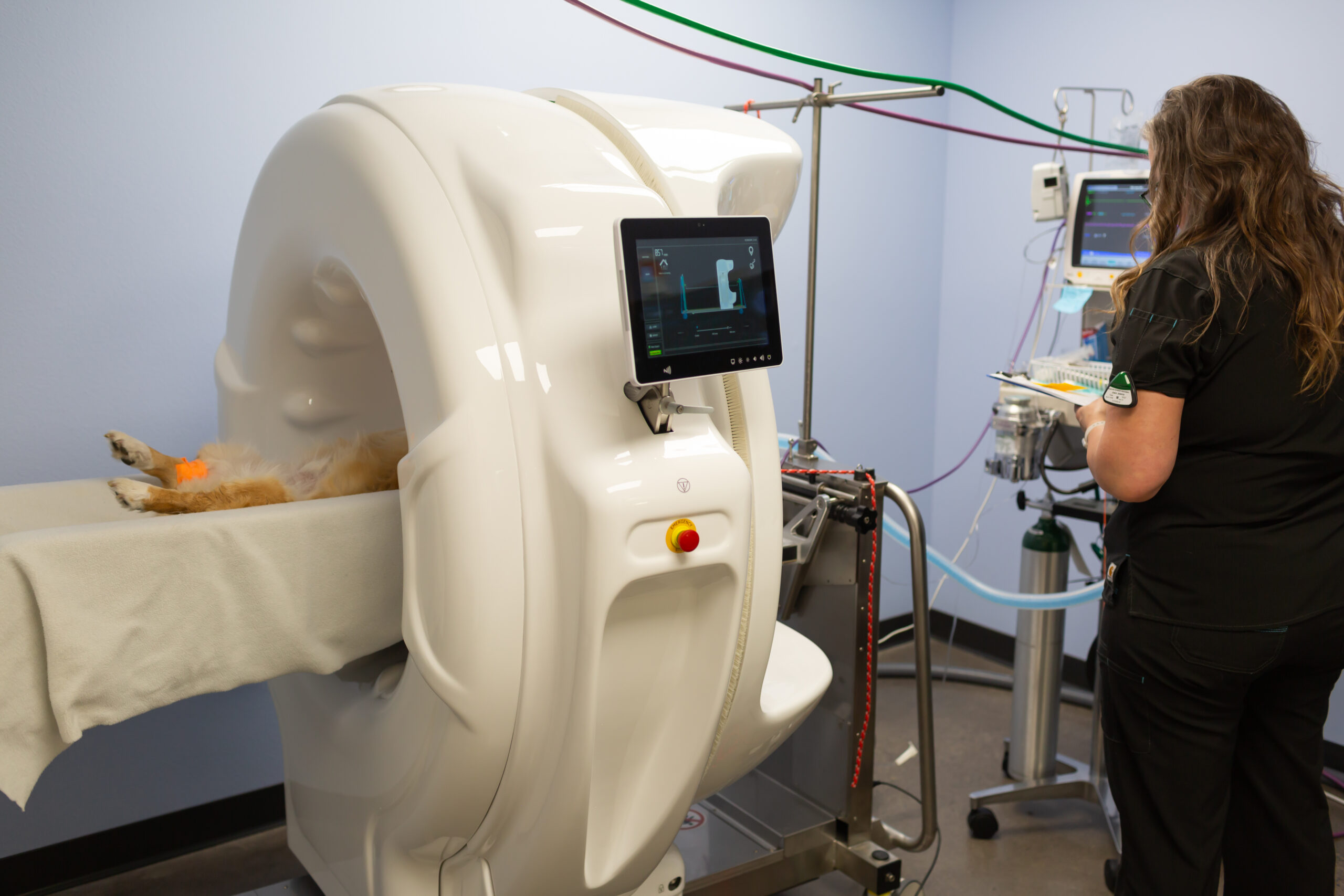
Introducing Advanced Imaging for Pets: What Makes HDVI Special? At Sunstone Veterinary Specialists, we are thrilled to introduce a groundbreaking imaging technology to our community: HDVI for pets....

Sunstone Updates, Tests and Procedures
In the last installment of our blog, we introduced you to one of our favorite diagnostic tools- endoscopy! We went over the basics and talked about gastrointestinal endoscopy,...

Sunstone Updates, Tests and Procedures
Welcome to the next installment of the Sunstone Vets Blog! This week, we will be talking about one of our favorite, minimally invasive diagnostic tools…..endoscopy! Endoscopy is a...

Tests and Procedures
If you are reading this blog, your pet has likely been advised to have an abdominal ultrasound for some type of health issue they are having. So,...
Overnight care available for hospitalized patients every night.
*Please call ahead 503-505-7255